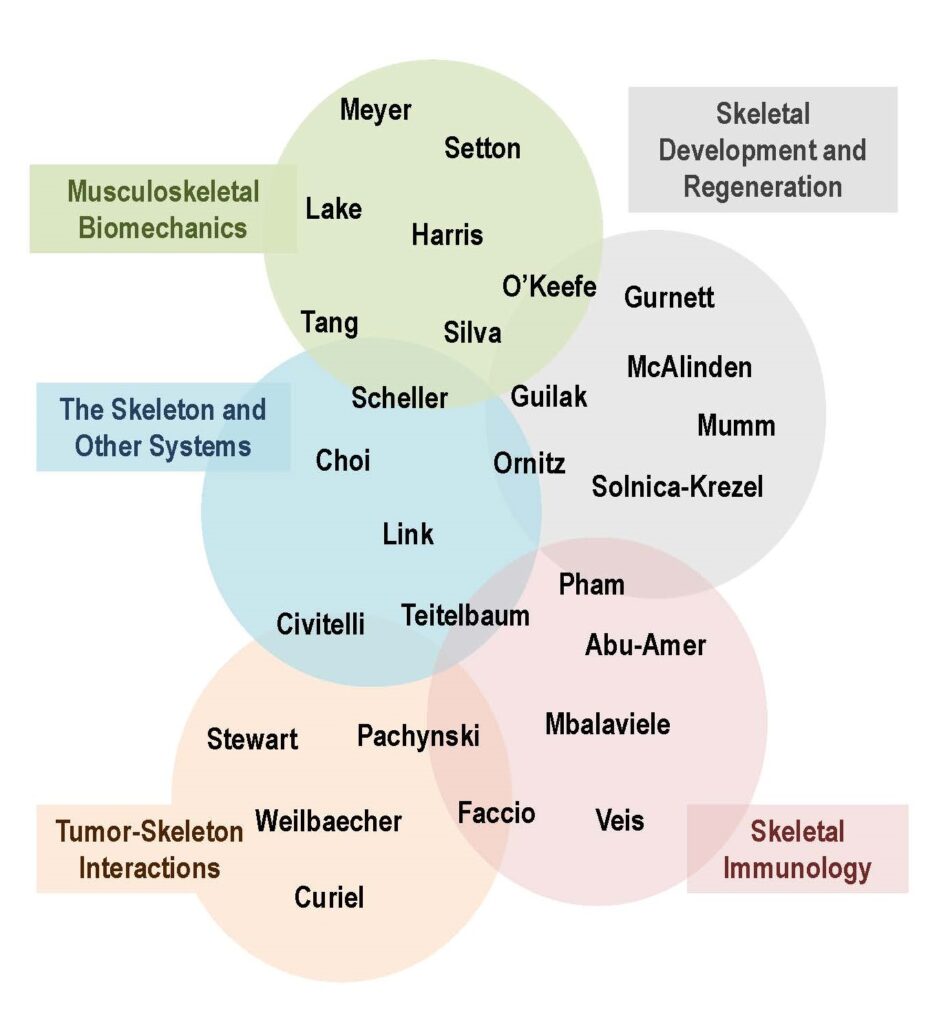
The five themes of the Skeletal Disorders Training Program (SDTP) represent the main focus of the faculty participating in this training program and are intended to provide context for applicants, highlighting common interests and interactions within each theme. Indeed, based on such interactions and shared interests, some faculty overlap more than one theme.
STDP faculty mentors are drawn from two schools and nine academic departments throughout the university:
- Biomedical Engineering
- Cell Biology and Physiology
- Developmental Biology
- Medicine
- Orthopaedic Surgery
- Pathology and Immunology
- Neurology
- Radiation Oncology
- Physical Therapy
They also represent a wide range of research interests:
The laboratories of 14 of our 28 mentors are housed in the Musculoskeletal Research Center (MRC) premises, greatly facilitating interactions; furthermore, the School of Medicine enjoys a single, physically interconnected campus that contains the laboratories of all mentors.
The SDTP has fostered a culture of collegiality and interactivity among our faculty, which is attested by co-authorship in publications, participation in the many educational activities of this program, and frequent service by SDTP mentors on thesis or advisory committees of SDTP and other MRC trainees, interactions that have also facilitated entry of new faculty into skeletal biology.
Choosing a Mentor
Our large mentor pool offers a wide range of research training opportunities, both pre-doctoral and post-doctoral, within the SDTP’s five thematic areas.
Pre-doctoral trainees may have a general idea of the research area they would like to pursue but insufficient knowledge of the human resources and mentorship opportunities available through this program.
To help students make the most appropriate choice of mentor and to encourage interactions, the Division of Biology & Biomedical Sciences (DBBS) and Department of Biomedical Engineering (BME) require PhD or MD/PhD students to undergo two to three 3-month-long rotations in different laboratories during their first year of training, before choosing their thesis mentor, and are typically appointed to this program in their second year.
After earning candidacy for graduation, pre-doctoral trainees form a Thesis Committee (TC), which must include the mentor and conform to program requirements. Likewise, BME students assemble thesis committees composed primarily of, though not exclusively limited to, BME faculty, and follow the same evaluation procedures as DBBS students.
Since applicants for post-doctoral positions typically have specific orientation towards a certain mentor or laboratory at the time of application, they are not required to rotate in other labs.
Within 6 months of appointment, post-doctoral trainees assemble a Training Advisory Committee (TAC), constituted by four faculty chosen by the trainee from among the program mentors (or other faculty whose expertise more closely aligns with the research topic), and including the trainee’s mentor.
The scope of this committee is similar to that of a pre-doctoral student thesis committee and is designed to provide additional guidance to the trainee towards achieving the goals of the research project and fulfill all the requirements of the training program. These advisory committees serve a crucial role in the trainee’s scholarly development within this program, and their feedback to the trainee and mentor is a fundamental component of the trainee’s yearly evaluation.
Mentors by Thematic Area
This group focuses on how bone cells are regulated by hormones and local factors and by interactions with other systems, such as hematopoietic, vascular and nervous systems, as well as the cross-regulation of skeletal homeostasis and energy metabolism.
Kyunghee Choi, PhD, Associate Professor of Pathology & Immunology
- Graduate Program Affiliations: Immunology; Molecular Cell Biology; Developmental, Regenerative and Stem Cell Biology, Cancer Biology
- Training Record and Ongoing Activities: Choi studies molecular mechanisms that regulate hematopoietic and vascular development and regeneration in the context of skeletal diseases; and in particular, hematopoiesis in chronic diseases in relation to changes in bone marrow microenvironment. Current research includes analysis of hematopoietic changes in chronic inflammatory diseases and cancer, and analysis of bone marrow microenvironment in chronic inflammatory diseases. Choi has trained 15 graduate students and post-doctoral fellows.
Roberto Civitelli, MD, Shoenberg Chair in Medicine, Professor of Orthopaedic Surgery and Cell Biology & Physiology
- Graduate Program Affiliations: Molecular Cell Biology; Molecular Genetics and Genomics
- Training Record and Ongoing Activities: Civitelli’s research interests include bone and mineral metabolism in health and disease, both at the clinical and basic science levels. He investigates the role of connexins in bone modeling, response to mechanical loading, and energy metabolism. New research directions address the role of cadherins in the tumor microenvironment and the role of Wnt signaling in diabetic bone disease. He has trained many graduate and undergraduate students (2 DBBS students graduated in the past 7 years) and postdocs and maintains an active clinical practice in osteoporosis and metabolic bone diseases.
Daniel Link, MD, Wolff Professor of Medicine and Pathology & Immunology
- Graduate Program Affiliations: Immunology; Molecular Cell Biology, Cancer Biology
- Training Record and Ongoing Activities: Link studies mechanisms regulating normal and malignant hematopoiesis, with particular interest in stromal cells that comprise hematopoietic niches in the bone marrow. Active research programs focus on defining the signals that regulate bone marrow stromal cells under basal and stress conditions, and those generated by stromal cells that regulate hematopoietic stem/progenitor cells. These studies have led to productive interactions with other SDTP faculty, including Drs. Civitelli, Teitelbaum, and Mbalaviele, offering a truly interdisciplinary approach to bone marrow biology with a strong translational angle. Link is Co-Director of the Hematopoiesis Development and Malignancy Program of the Siteman Cancer Center. He has a very strong mentoring record, with 13 graduate students and 22 post-doctoral fellows trained in his lab in the past 10 years.
Erica Scheller, DDS, PhD, Assistant Professor of Medicine and Cell Biology & Physiology
- Graduate Program Affiliation: DBBS: Developmental, Regenerative and Stem Cell Biology; Molecular Cell Biology; Neurosciences. BME: Molecular & Cellular Systems Engineering; Biomedical & Biological Imaging; Neural Engineering; Orthopaedic Engineering; Regenerative Engineering in Medicine.
- Research Area and Ongoing Activities: Scheller synthesizes concepts from cell biology, physiology, and bioengineering to study the relationships between the nervous system and the skeleton. The Scheller lab is interested in understanding how neural signals contribute to skeletal homeostasis, and how perturbations to this system contribute to changes in local energy metabolism and adiposity, impaired regeneration, and skeletal fragility in states of health and disease. They take a bench-to-bedside approach to research and leverage molecular biology, high-resolution imaging, rodent models, and human studies to pursue translational mechanistic studies from bone to brain. Scheller has developed a strong training record, mentoring 3 postdocs and 2 graduate students, including two SDTP trainees.
This group studies the interactions between the immune system and the skeleton. This research theme remains a core interest of this program, spanning translational and clinical studies on non-malignant disorders involving abnormal osteoclast activation.
Yousef Abu-Amer, PhD, Key Professor of Orthopaedic Surgery and Cell Biology & Physiology
- Graduate Program Affiliation: DBBS: Molecular Cell Biology; Developmental, Regenerative and Stem Cell Biology
- Training Record and Ongoing Activities: Abu-Amer investigates the molecular mechanisms underlying degenerative skeletal diseases such as inflammatory arthritis, joint degeneration, and osteolysis. Using tissue-specific gene deletions and expression approaches, Abu-Amer has delineated the role of various components of the NF-B transcription factor family in skeletal development, joint and bone pathologies, and the role of NF-B as a link between intestinal inflammation and skeletal wasting, synovial inflammation and joint destruction. His long term goal is to identify signal-specific targets to enable tissue-selective intervention to inhibit breakdown of skeletal elements and spare off-target effects. He has trained 1 pre- and 4 post-doctoral trainees in the past 10 years.
Gabriel Mbalaviele, PhD, Professor of Medicine
- Graduate Program Affiliation: DBBS: Molecular Cell Biology; Developmental, Regenerative and Stem Cell Biology
- Training Record and Ongoing Activities: Mbalaviele focuses on the role of the inflammasomes in bone biology and disease; and the role of PARP1 in osteoclastogenesis. Using pharmacological tools and mouse genetic models, his research elucidates the cellular and molecular networks through which sterile inflammation impacts skeletal homeostasis, with the goal of designing new therapeutic strategies for inflammatory skeletal disorders. Before joining Washington University School of Medicine, Mbalaviele spent 13 years in the pharmaceutical industry, developing drugs to treat autoimmune and autoinflammatory diseases. Mbalaviele has trained 3 post-doctoral fellows, including one SDTP trainee.
Christine Pham, MD, PhD, Professor of Medicine and Pathology & Immunology
- Program Affiliation: DBBS: Immunology; Molecular Genetics & Genomics
- Training Record and Ongoing Activities: Pham studies the contribution of innate and adaptive immunity to inflammatory conditions, including rheumatoid arthritis and osteoarthritis. Her laboratory is also developing strategies to deliver nanomedicines and bioengineered stem cells to halt or reverse joint degeneration in preclinical models of these disorders. Pham serves as Chief of the Division of Rheumatology, and Director of the WU Rheumatic Diseases Research Resource-based Center (RDRRC). In the past 10 years, Pham has trained 8 post-doctoral fellows.
Deborah Veis, MD, PhD, Professor of Medicine and Pathology & Immunology
- Graduate Program Affiliation: DBBS: Molecular Cell Biology; Immunology; Molecular Microbiology and Microbial Pathogenesis
- Training Record and Ongoing Activities: Veis studies alternative NF-κB and mitochondrial dynamics in osteoclasts and osteoblasts, using genetically modified animal models. Another are of interest is osteomyelitis, focusing on the interactions of pathogens such as S. aureus with cells in the bone microenvironment. As a board-certified pathologist with expertise in bone, Veis also collaborates with clinicians on studies related to bone disease and bone metastasis. Veis’s training record includes 3 predoctoral trainees, including 2 in SDTP students, and 5 postdocs.
Steven Teitelbaum, MD, Messing Professor of Pathology & Immunology and Medicine
- Graduate Program Affiliation: DBBS: Molecular Cell Biology; Developmental, Regenerative and Stem Cell Biology
- Research Area and Ongoing Activities: Teitelbaum’s works to delineate mechanisms of osteoclastic bone resorption and has recently extended his interests to the interactions between bone, fat and energy metabolism. Current research interests include determining the relationship of adiposity and bone, and exploring the ability of genetically modified myeloid lineage cells to prevent inflammatory arthritis and osteoarthritis. Teitelbaum is a world leading bone biologist and has trained more than 70 graduate students and fellows, including some of the mentors of this program (Drs. Abu-Amer, Faccio, and Veis).
These scientists are focused on the molecular mechanisms by which breast cancer and other solid tumors metastasize to the bone, and the role of the bone microenvironment in driving tumor growth and metastasis.
David Curiel, MD, PhD, Professor of Radiation Oncology
- Graduate Program Affiliation: DBBS: Molecular Microbiology and Microbial Pathogenesis
- Training Record and Ongoing Activities: Curiel is interested in gene therapy in a variety of conditions, focusing on the development of vectors capable of efficient and specific gene delivery to target cells through genetic engineering of recombinant adenovirus vectors, testing applications for modulating the tumor microenvironment and tissue engineering. Curiel brings unique expertise in a growing area of research highly relevant to skeletal metastasis. He has a strong record of training, having served as Director of a T32 program on cancer gene therapy, and has mentored more than 30 graduate students and post-docs in the past 15 years.
Roberta Faccio, PhD, Professor of Orthopaedic Surgery and Cell Biology & Physiology
- Graduate Program Affiliation: DBBS: Molecular Cell Biology; Immunology
- Training Record and Ongoing Activities: Faccio investigates how aberrant immune function modulates tumor growth in bone, as well as the adaptive and innate immune responses during inflammatory arthritis, in particular focusing on myeloid derived immune suppressive cells. Faccio has mentored 2 PhD students, one of whom was a SDTP trainee and 11 post-doctoral fellows. Notably, Faccio has been a member of the admissions and steering committees for the DBBS Molecular and Cell Biology graduate program, and in January 2020, she was appointed as Director of the Molecular and Cell Biology program.
Russell Pachynski, MD, Assistant Professor of Medicine, Division of Oncology
- Graduate Program Affiliation: None
- Training Record and Ongoing Activities: Although broadly focused on tumor immunology and leukocyte trafficking, Pachynski was appointed to the SDTP in 2018 based on his clinical and research focus in prostate cancer. In collaboration with Dr. Weilbaecher, the Pachynski lab has established fully immunocompetent models of bone metastatic prostate cancer, and with other groups, they have developed advanced imaging modalities to serially assess disease progression. Pachynski has identified a novel innate chemoattractant, chemerin, as a tumor suppressive cytokine, and is now pursuing its development as a therapeutic target. Pachynski has trained 8 pre-doctoral and 2 post-doctoral students.
Sheila Stewart, PhD, Professor of Cell Biology & Physiology
- Graduate Program Affiliation: DBBS: Molecular Cell Biology; Molecular Genetics and Genomics; Biochemistry; Computational and Systems Biology; Cancer Biology
- Training Record and Ongoing Activities: Stewart studies how age-related changes in the tumor microenvironment contribute to tumorigenesis. She has identified a senescence associated secretory phenotype that increases local osteoclastogenesis and tumor cell seeding to regions with senescent osteoblasts. Dr. Stewart has served on 30 thesis committees as well as on the DDBS Molecular and Cellular Biology Steering Committee, Genetics Steering Committee and Admissions Committee. She is also director of the newly formed Cancer Biology PhD Program. Dr. Stewart has mentored 8 PhD students, 4 post-doctoral fellows and many undergraduate students.
Katherine Weilbaecher, MD, Langenberg Professor of the Science and Practice of Medicine
- Graduate Program Affiliation: DBBS: Molecular Cell Biology; Molecular Genetics and Genomics
- Training Record and Ongoing Activities: Weilbaecher is a physician-scientist who studies the molecular basis of tumor reprogramming of the bone microenvironment. Current activity focuses on the role of the β3 integrin signaling in the process of bone metastasis, pathologic bone loss, HTLV-1 adult T-cell leukemia and multiple myeloma bone marrow colonization. As a practicing breast cancer medical oncologist at the WU Siteman Cancer Center, Weilbaecher has developed 4 clinical trials to prevent and treat breast cancer bone metastases directly resulting from her laboratory research. Therefore, her laboratory is an ideal environment to train future translational researchers. She has mentored hematology fellows, MD/PhD students and post-doctoral fellows with basic research projects into the mechanisms of bone metastasis, including 2 SDTP trainees.
This group of investigators explores the effects of mechanical and metabolic factors on bone, cartilage, tendons, intervertebral disc and muscle.
Michael Harris, PhD, Assistant Professor of Physical Therapy and Orthopaedic Surgery
- Graduate Program Affiliation: Movement Science (Program in Physical Therapy) ; Biomedical Engineering; Mechanical Engineering
- Training Record and Ongoing Activities: Dr. Harris’ research links outward manifestations of orthopaedic pathology (e.g. functional deficits) with internal abnormalities (e.g. skeletal deformity, muscle dysfunction). His current NIH-funded research uses in-vivo biomechanics, medical imaging, and musculoskeletal modeling to study mechanisms of damage and consequences of treatment for hip dysplasia. Dr. Harris teaches biomechanics coursework in the programs of Movement Science, Physical Therapy, and Biomedical Engineering. He has trained 1 pre-doctoral student in Mechanical Engineering and 1 post-doctoral fellow. He currently mentors 2 pre-doctoral students in Movement Science, 2 undergraduate students in Biomedical Engineering, and 2 Doctorate of Physical Therapy students.
Spencer Lake, PhD, Associate Professor of Mechanical Engineering & Materials Science, Orthopaedic Surgery, and Biomedical Engineering
- Graduate Program Affiliation: BME: Orthopaedic Engineering; Regenerative Engineering in Medicine
- Training Record and Ongoing Activities: Lake’s research focuses on multiscale structure-function relationships of musculoskeletal soft tissues and joints. His group studies tendons and ligaments to understand how these tissues function in healthy conditions and in response to injury, elucidating constituents of connective soft tissues that contribute to transferring load/strain across the hierarchical levels of tendon, particularly elastin and elastic fibers. They also study tissue fibrosis in the context of post-traumatic joint contracture of the elbow and seek to develop improved treatment strategies for this debilitating condition. He has mentored 6 pre-doctoral and 2 post-doctoral trainees, and is currently mentoring one SDTP pre-doctoral trainee.
Gretchen Meyer, PhD, Assistant Professor of Physical Therapy, Neurology, Biomedical Engineering, and Orthopaedic Surgery
- Graduate Program Affiliation: DBBS: Developmental, Regenerative and Stem Cell Biology Program and Biomedical Engineering; BME: Molecular & Cellular Systems Engineering; Orthopaedic Engineering; Regenerative Engineering in Medicine
- Training Record and Ongoing Activities: Meyer is the founder and current director of the Integrative Muscle Physiology laboratory. Her research focuses on the role of inter- and intra-muscular adipose tissue in skeletal muscle biomechanics and physiological function, offering unique training opportunities in muscle physiology, cell biology and biomechanics. Her overarching hypothesis is that in conditions of orthopaedic injury (i.e. rotator cuff tears) and disease (i.e. type 2 diabetes) where intra-muscular adipose tissue expands dramatically, fat-muscle cross-talk has become deranged and impedes muscle regeneration, compromising force transmission to the tendon and skeleton. Meyer has trained 2 pre-doctoral students.
Regis O’Keefe, MD, PhD, Reynolds Professor of Orthopaedic Surgery
- Graduate Program Affiliation: DBBS: Molecular Cell Biology; Molecular Genetics and Genomics
- Training Record and Ongoing Activities: O’Keefe’s research addresses skeletal biology and regeneration. One focus is on the role of epigenetics (DNA methylation) in cartilage energy metabolism and the balance of anabolic and catabolic gene expression in articular cartilage. The laboratory has identified 4-aminobutuyric acid transferase as a key target regulating mitochondrial energy metabolism in the pathogenesis of osteoarthritis. In the area of bone regeneration, the laboratory is interested in the cellular signals that regulate periosteal progenitor cells in the context of bone repair, particularly cyclooxygenase. O’Keefe is also a practicing surgeon, specialized in the management of bone and soft (connective) tissue tumors, skeletal reconstruction, and primary and revision total hip and knee arthroplasties. As a successful physician-scientist and accomplished teacher with numerous previous trainees, O’Keefe has mentored one SDTP post-doctoral trainee.
Lori Setton, PhD, Lopata Professor of Biomedical Engineering, Orthopaedic Surgery, and Mechanical Engineering & Materials Science
- Graduate Program Affiliation: DBBS: Developmental, Regenerative and Stem Cell Biology; Molecular Cell Biology Program; BME: Orthopaedic Engineering; Regenerative Engineering in Medicine
- Training Record and Ongoing Activities: Setton’s research focuses on understanding the mechanisms for degeneration and regeneration of soft tissues of the musculoskeletal system, and their contribution to pain‐related dysfunction. Recent work has focused on development of in situ forming hydrogels for drug and cell delivery to the intervertebral disc and knee joints to attenuate development and symptoms associated with disc degeneration and arthritis. Setton has directly supervised 22 pre-doctoral and 23 post-doctoral trainees, as well as numerous undergraduate students.
Matthew Silva, PhD, Peterson Professor of Orthopaedic Surgery and Biomedical Engineering
- Graduate Program Affiliation: DBBS: Molecular Cell Biology; Human and Statistical Genetics; BME: Orthopaedic Eng; Regenerative Eng in Medicine
- Training Record and Ongoing Activities: Silva’s research interest is on the development, injury, repair and mechanobiology of musculoskeletal tissues, particularly bone. He is an expert in biomechanics and finite element analysis. Current research projects address the osteogenic and angiogenic responses to bone injury, and the response of the osteoporotic skeleton to mechanical loading. Silva offers unique and much sought-after expertise to the skeletal biology research community and directs the P30 that supports the MRC infrastructure. In the past 10 years, he has trained 7 PhD students and 6 post-doctoral fellows, including 5 SDTP trainees.
Simon Tang, PhD, MSCI, Associate Professor of Orthopaedic Surgery
- Graduate Program Affiliation: DBBS: Biochemistry, Biophysics & Structural Biology; BME: Orthopaedic Engineering; Regenerative Engineering in Medicine
- Training Record and Ongoing Activities: With the overall theme of understanding the biological regulation of skeletal matrix quality, Tang’s research group integrates engineering and biology approaches for understanding the effect of disease mechanisms on the structure-function relationships of skeletal tissues and developing translatable therapeutic and regenerative strategies for these diseases. Current projects span intervertebral disc degeneration, low back pain, and tissue engineering. The interdisciplinary nature of Tang’s laboratory has attracted 6 trainees, including one SDTP post-doc.
This group includes investigators from different disciplines whose common interest is the genetic bases of skeletal disorders, skeletal development and regeneration. Research spans pre-clinical model systems, including zebrafish (a new addition) and mouse, as well as human genetics.
Farshid Guilak, PhD, Simon Professor of Orthopaedic Surgery, Biomedical Engineering, and Developmental Biology
- Graduate Program Affiliation: DBBS: Developmental, Regenenerative & Stem Cell Biology, Molecular Cell Biology; Immunology; BME: Molecular & Cellular Systems Eng; Orthopaedic Eng; Regenerative Eng in Medicine
- Training Record and Ongoing Activities: By combining principles of engineering and developmental biology, the Guilak laboratory deconstructs the processes that drive joint development and function, and then aims to reconstruct and even improve these processes using custom-designed stem cells and biomaterials. They employ adult mesenchymal, adipose-derived, and induced pluripotent stem cells, as well as new methods in synthetic biology and genome engineering to create “designer” stem cells with built-in gene circuits to allow autoregulated responses to environmental signals, such as inflammation. With Lilianna Solnica-Krezel, PhD, he co-directs the Center of Regenerative Medicine. Guilak is a highly experienced mentor, having supervised over 56 predoctoral students and 36 postdoctoral fellows, including 3 SDTP post-doctoral trainees.
Christina Gurnett, MD, PhD, Professor of Neurology
- Graduate Program Affiliation: DBBS: Human & Statistical Genetics
- Training Record and Ongoing Activities: Gurnett is a clinician scientist expert in genetics. Her laboratory focuses on genomic discovery of pediatric musculoskeletal disorders and understanding how genetic variation results in disease. Her interests span the development of high-throughput functional genomic methods using single cells, as well as modeling of human disease in zebrafish. Of relevance to this program, in collaboration with Solnica-Krezel, Gurnett has developed zebrafish models to study clubfoot, scoliosis and other neurodevelopmental disorders. Gurnett is Director of the Division of Pediatric and Developmental Neurology, Associate Director of the ICTS, and Co-Director of the Institute of Intellectual and Developmental Disabilities Research Center. In the past 10 years she has trained 3 PhD students and 8 post-doctoral fellows.
Audrey McAlinden, PhD, Associate Professor of Orthopaedic Surgery, Cell Biology & Physiology and Biomedical Engineering
- Graduate Program Affiliation: DBBS: Developmental, Regenerative and Stem Cell Biology; BME: Molecular and Cellular Systems Engineering
- Training Record and Ongoing Activities: McAlinden focuses on mechanisms regulating skeletal (cartilage and bone) development as a means to discover new strategies to treat orthopaedic conditions. Current research seeks to understand how microRNAs and long non-coding RNAs modulate chondrogenesis and osteogenesis. She investigates the potential therapeutic benefit of targeting specific microRNAs in vivo, using clinically relevant mouse models of bone fracture repair, heterotopic ossification and osteoarthritis. McAlinden has mentored 2 trainees, including one SDTP post-doc; and coordinates the SDTP Mock Study Sections
Steven Mumm, PhD, Professor of Medicine
- Graduate Program Affiliation: None
- Training Record and Ongoing Activities: The focus of Mumm’s research is the molecular genetics of metabolic bone diseases and skeletal dysplasias, in conjunction with Michael Whyte, MD, a world-leading authority in metabolic bone disorders and senior faculty in the Division of Bone and Mineral Diseases. Mumm’s lab focuses on new disease gene discovery and genotype/phenotype correlations for diseases where access to a large number of patients is possible. Current activity involves development of new zebrafish models and induced pluripotent stem cells from rare disease patients to study the mechanisms of these disorders. Dr. Mumm hosts summer students in the Students and Teachers as Research Scientists (STARS) Program, aimed at attracting a diverse array of high school students to science.
David Ornitz, MD, PhD, Alumni Endowed Professor of Developmental Biology
- Graduate Program Affiliation: DBBS: Developmental, Regenerative and Stem Cell Biology; Molecular Cell Biology; Neuroscience
- Training Record and Ongoing Activities: Ornitz’s research focuses on the role of Fibroblast Growth Factor Receptor (FGFR) signaling in the regulation of osteocyte viability and skeletal homeostasis in adult and aging bone. Current efforts are on identifying novel molecular pathway interactions with FGFR signaling in osteoblasts and osteocytes, evaluating potential adverse effects of an FDA approved FGFR inhibitor on bone. Other projects are focused on identifying new genes and pathways that could be targeted to promote skeletal homeostasis. Ornitz has trained more than 20 postdoctoral fellows in the past 10 years.
Lilianna Solnica-Krezel, PhD, Professor of Developmental Biology
- Graduate Program Affiliation: DBBS: Developmental, Regenerative & Stem Cell Biology; BME: Biomedical & Biological Imaging; Molecular & Cellular Systems Engineering
- Training Record and Ongoing Activities: Solnica-Krezel was also recently appointed to the program. Using genetic, genomic and proteomic approaches in zebrafish and embryonic stem cells, Solnica-Krezel’s laboratory investigates how these processes are coordinated to ensure normal development and contribute to human disease. They use a forward genetic approach to identify adult zebrafish mutants with spinal deformities, and reverse genetics to validate candidate scoliosis genes identified by genetic and genome wide association studies. Solnica-Krezel has trained 17 PhD students, 14 of whom continued training as postdocs and 4 hold academic positions. Likewise, 10 of her former 20 postdoctoral trainees have independent tenure track positions in academia